"It’s dark by the river when it’s night in the forest, |
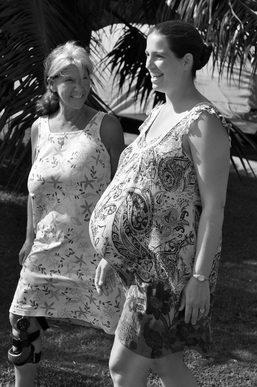
In honor of Jill, an incredibly strong mother
The call phone rings, sleep recedes
Answer hushed, try not to disturb
Throw on clothes, creep down stairs,
Flick on lights, grab the baggage,
heavier than preferred.
Miles apart, both midwives pack
Their cars in duplicate,
Each enough to stand alone,
Intended to be together, yet
ready just in case.
Baggage is unpacked, organized,
Touch brings memory of use,
The watching begins: quiet, unobtrusive,
Always with prayer for wisdom and
insight to serve well.
Labor blossoms with patience-
Power, passage, passenger, psyche-
Orchestrated to a climax where
Mother is transformed as
her babe emerges.
Many times the baggage remains
As heavy at departure
As upon arrival.
But other days ...
Watchful eyes spy a need,
Listening ears hear a call for help,
Agile hands sift through supplies,
utilizing tools appropriate.
Today the baggage contents-
Combined with inspiration, intelligence, intuition-
Sufficed for safe passage.
Never taken for granted, prayers are lifted
with profound gratitude.
Upon departure, the heavy baggage
Is no longer so.
Realization sets in.
All is needful, despite being
heavier than preferred.
© 2023 Chloe Raum. All rights reserved.
The call phone rings, sleep recedes
Answer hushed, try not to disturb
Throw on clothes, creep down stairs,
Flick on lights, grab the baggage,
heavier than preferred.
Miles apart, both midwives pack
Their cars in duplicate,
Each enough to stand alone,
Intended to be together, yet
ready just in case.
Baggage is unpacked, organized,
Touch brings memory of use,
The watching begins: quiet, unobtrusive,
Always with prayer for wisdom and
insight to serve well.
Labor blossoms with patience-
Power, passage, passenger, psyche-
Orchestrated to a climax where
Mother is transformed as
her babe emerges.
Many times the baggage remains
As heavy at departure
As upon arrival.
But other days ...
Watchful eyes spy a need,
Listening ears hear a call for help,
Agile hands sift through supplies,
utilizing tools appropriate.
Today the baggage contents-
Combined with inspiration, intelligence, intuition-
Sufficed for safe passage.
Never taken for granted, prayers are lifted
with profound gratitude.
Upon departure, the heavy baggage
Is no longer so.
Realization sets in.
All is needful, despite being
heavier than preferred.
© 2023 Chloe Raum. All rights reserved.


 RSS Feed
RSS Feed